
Vlad Dzhashi, MD
I wanted to try telemedicine for a while and although I’d been slammed with emails and phone calls trying to sign me up for outpatient gigs, telehospitalist jobs seemed to be few and far between.
Luckily, I work at a local hospital system that is one of the telehospitalist pioneers in the US.
They created both telehospitalist and tele-ICU programs from scratch a few years ago. Both are fully functioning at five regional hospitals and expanding now.
I wanna say, it wasn’t easy to get on schedule, since VirtualMD positions (i.e., telehospitalist) are always in high demand and there are rarely any openings. After a few attempts, I was finally scheduled for four nights.
Today, I wanted to share my experience and give you a glimpse of what hospital medicine may look like in the near future.
Click here to download my FREE report: see who’s currently hiring telehospitalists
TeleHospitalist set up
Where?
Unlike many other telemedicine jobs, I didn’t work from home. The hospital provided a separate office space for the telemedicine team.
Hours:
I worked 11.5 hour shifts, which started at 8:30 pm and ended at 8:00 am.
My workplace:
One thing I absolutely loved was my super crazy sci-fi display setup: there were six monitors, with each of them having its own purpose.
With this setup, I had all the info available on one of the screens, including EKG’s, EMR, Uptodate, etc.
Another absolutely cool thing that blew my mind was that some of the patients’ rooms (PCU and ICU) were equipped with cameras so I could get connected and eyeball these patients “virtually.”
On top of that, the desk’s height was adjustable with a push of a button; you could move it up or down and you could raise it to make it a standing desk. Although I was stuck in a chair for the duration of the shift, my teammates kept switching between sitting and standing every couple of hours to prevent DVT.
The Team:
I had two “partners” in crime: RN and NP, so all the calls/messages were distributed equally. Having said that, I was the only one doing admits.
Responsibilities/Workload
1 – Cross Coverage: responding to the calls from hospital nurses across five hospitals.
The team receives all the messages into a special email folder that is updated real-time.
The RN would take the easiest calls: prn sleep meds, prn laxatives, ordering morning labs, etc. A lot of the orders were by default, so she would not need to discuss them with an MD or NP.
Our RN would also help with admin stuff, e.g., getting ahold of a certain floor or a particular service department in the hospital: e.g., lab, microbiology, blood back, etc.
The MD and NP took care of all the other more complicated calls, although the MD was responsible for ICU calls most of the time.
What were the most common calls/messages we would see?
Hypotension, low H&H, other critical lab results, tachycardia/bradycardia, pain meds, patient requesting to leave AMA (my favorite: Really? At 2 am? Don’t you want to sleep?).
Volume:
The average number of calls the telehospitalist team would “process” was close to 300.
Interestingly enough, there were a few very busy times at night:
Evenings when RNs changed shifts, then 4-5 am when morning labs were back, with a third peak around 7-8 am when morning shifts started.
The time between 1-3 am was a little slow, so I managed to take short naps.
Liability and documentation:
Of course, the liability part is there even if you cover patients virtually.
Think about it: as a telemedicine hospitalist, I was covering almost 500+ very sick patients, some of them in ICU’s.
I came up with my own strategy to provide better “virtual” patient care for the patients and to minimize the liability:
First of all, almost every time I got a message, I picked up a phone and talked to the nurse to clarify the patient’s status and ask questions. I would also glance at the last hospitalist progress note to get a better understanding of what was going on with the patient.
This approach made a big difference, as I caught myself changing my orders after talking to the nurse and reviewing the chart multiple times.
Second, I would also put a note in the chart, documenting what info I’d gotten from the nurse and what new orders or changes I’d made.
These notes were also important for day hospitalists to make sense of what actually happened with the patient overnight.
Now, you may be wondering what if a patient were too sick and needed to be evaluated?
When this situation came up, I would call an in-house doc and ask him to lay eyes and hands on the patient.
2 – TeleHospitalist Admissions:
One of the hospitals I was covering was a tiny critical access and rehab facility that didn’t have an in-house nocturnist.
I was responsible for admits that would come overnight as well as for covering their rapid responses and codes. (There was also an ER doc who was physically present at night and who would help with codes if needed.)
I would first receive a call from the ER doc, discuss the patient’s case, and if I accepted, I would put admission orders in.
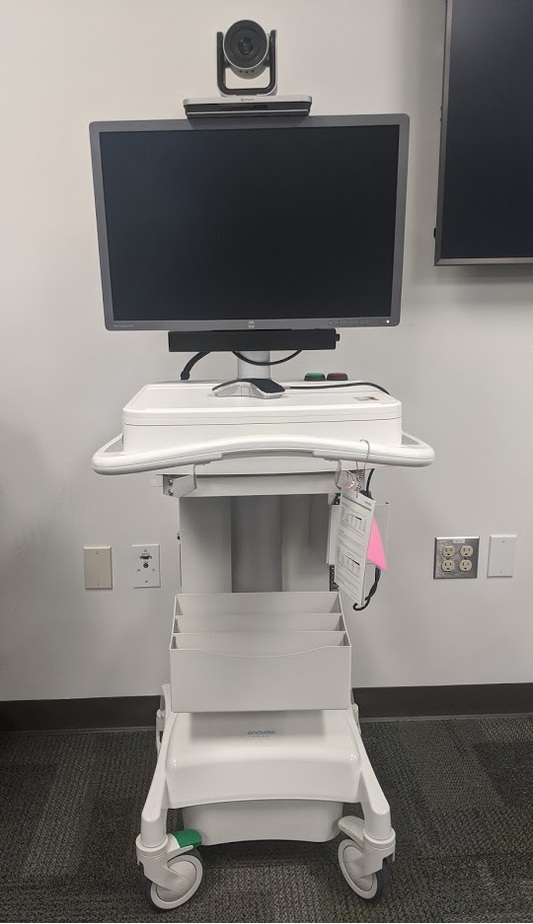
Once a patient reached the floor (this would take an hour or two), the RN would message me and I would connect to the telemedicine cart.
The cart had a camera on top that I could control as well as an attached stethoscope.
I would interview the patient and then ask a bedside RN to help me with the exam.
Here’s how the physician exam worked:
First, I ask the RN to do palpation, shine the light into the patient’s eyes and mouth while zooming the camera on the patient. She would do a brief neuro exam.
Then I would ask the RN to use the attached stethoscope to auscultate lungs, heart and abdomen, which I would hear in my headphones.
This way, the physical exam took about five minutes longer than it would normally take.
At the end, I would disconnect and complete my H&P and add orders if needed.
Final Verdict
Overall, telehospitalist night coverage is a win-win:
1 – It unloads night hospitalists – all they need to do is to stay focused on admission and codes/rapid responses. It keeps your nocturnists’ morale high and surely prevents burnout.
2 – This is great from the patients’ and nurses’ perspective: they get more timely responses, unlike when your night doc is juggling between admits and floor calls.
3 – Also, since all the virtual/telemedicine team does is the cross-coverage, the patients receive more attention, providing better quality of care.
Things to improve:
I would definitely prefer to work as a telehospitalist from home. I don’t see any good reason why this cannot be done from the comfort of your home.
Another issue is that admissions take longer than live admits, and some patients would prefer to see the doctor at the bedside rather than virtually.
P.S. Now, I am turning to you. Let me know in the comments if you’ve done any telemedicine work and what your thoughts are. Is it Yay or Nay?
As featured on




New to locum tenens? Check out my complete guide for newbies in 2021!

sekolah tinggi ilmu kesehatan ukpm
kebidanan mitra sejahtera jakarta
akademi analis kesehatan muhammadiyah surabaya
akademi kesehatan lingkungan sumsel
akademi kebidanan arta kabanjahe
akademi kebidanan nusantara medan
akademi kebidanan delhus delmed
akper harapan mama deli serdang


Hi!, Sounds like you had a great time. Are you still doing this? I have more questions, let’s start with those first. Looking forward for your answer. Thanks!
Hi, Axia! What questions do you have?
How do you foresee Telemedicine and Long Distance Coverage for other specialties that are in need of “coverage”?
Also, advice on tech aspects of ensuring good match of ease of use ( as against the current EMR problems).
Thanks.
Andy Cheng
Hi, Andrew!
I think telemedicine is going to develop and more and more specilaties will be involved. Obsiously, surgical specilaties will be the last to join but it is only a matter of time before we’ll see “long’distance” surgeries using robots.
As to your second question, although EMR made telemedicine possible, but if you cover multiple hospitals with different EMR it is very challenging to do, so there’s definitely a room for improvement there.
How much does it pay?
Or if uncomfortable answering that directly, how much does it pay relative to normal hospitalist work?
Clearly, the hospital is saving shitloads of money this way.
Do you share in this wealth creation?
Also, i would worry about the inherent pressures to avoid sending someone physically to the patient.
Hi, Tha Schnookz!
It was paid $200/hr, which is the same rate all per-diem nocturnists make. As to the “pressure”, it does exist, it is somethimes tricky to decide. Having said that, in all of our hospitals, RNs can activate “rapid reponse” without asking a physician, so most of the time the “in-house” nocturnist will be called anyways.
Vlad.
Where can I find Telehospitalist opportunities?
Or better yet, let’s start our own company? I’m hospitalist physician and entrepreneur. Would love to talk to you more about it.
covering nocturnally as many as 65 patients and admitting as many as 16 patient is a 12 hour shift, certainly, the majority of phone calls can be handled without seeing the patient. Since a good portion of a HNP is history, that also does not require a physical presence. The actual exam, then becomes dependent on the assitant in the room, and your confidence in them, as well as the remote tools available- ie stethescope. Im interested
Thanks for helping me understand that tele-nocturnists would be responsible for the admissions overnight and the rapid responses and codes. I hope we can find one we can trust this evening, since we are concerned about my grandmother who has mobility issues. She just suddenly can’t move her one arm as well, so we want her to get checked right now.
If you don’t mind sharing, which company was this experience through. I am currently working as a nocturnist looking to break into the tele-nocturnist world next year. I have looked a many companies so far but all have vague descriptions and your explanation was far superior.
It was through the CHI Franciscan hospital system.